Gestational diabetes mellitus (GDM) affects between 2% and 5% of pregnant women. It is especially common during the last third of pregnancy. It affects 1% of those under the age of 20 and 13% of those over the age of 44. A number of ethnic groups including Asians, American Indians, Indigenous Australians, and Pacific Islanders are at higher risk. In 90% of people gestational diabetes will resolve after the baby is born. Women; however, are at an increased risk of developing type 2 diabetes. See the images:
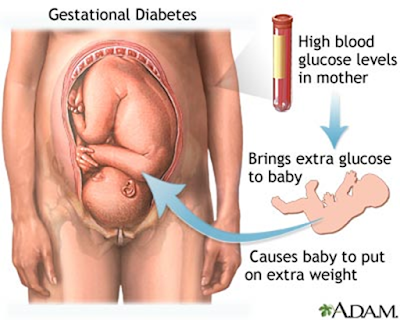
Insulin is a hormone whose job is to enable glucose (sugar) in the bloodstream to enter the cells of the body, where sugar is the source of energy. All fetuses (babies) and placentas (afterbirths) produce hormones that make the mother resistant to her own insulin.
Most pregnant women produce more insulin to compensate and keep their blood sugar level normal. Some pregnant women cannot produce enough extra insulin and their blood sugar level rises, a condition called gestational diabetes. Gestational diabetes affects between 5 and 18 percent of women during pregnancy, and usually goes away after delivery.
Insulin is a hormone whose job is to enable glucose (sugar) in the bloodstream to enter the cells of the body, where sugar is the source of energy. All fetuses (babies) and placentas (afterbirths) produce hormones that make the mother resistant to her own insulin.
Most pregnant women produce more insulin to compensate and keep their blood sugar level normal. Some pregnant women cannot produce enough extra insulin and their blood sugar level rises, a condition called gestational diabetes. Gestational diabetes affects between 5 and 18 percent of women during pregnancy, and usually goes away after delivery.
What is Gestational diabetes mellitus (GDM)?
Gestational diabetes mellitus (GDM) is defined as glucose intolerance of various degrees that is first detected during pregnancy. GDM is detected through the screening of pregnant women for clinical risk factors and, among at-risk women, testing for abnormal glucose tolerance that is usually, but not invariably, mild and asymptomatic.
GDM appears to result from the same broad spectrum of physiological and genetic abnormalities that characterize diabetes outside of pregnancy. Indeed, women with GDM are at high risk for having or developing diabetes when they are not pregnant.
Gestational diabetes mellitus (GDM) represents a heterogeneous group of metabolic disorders, which result in varying degrees of maternal hyperglycemia and pregnancy-associated risk. The frequency of GDM is rising globally and may also increase further as less-stringent criteria for the diagnosis are potentially adopted.
You may have a greater risk of developing gestational diabetes if you:
But half of women who develop gestational diabetes have no risk factors.
Gestational diabetes typically does not cause any noticeable signs or symptoms. This is why screening tests are so important. Rarely, an increased thirst or increased urinary frequency may be noticed.
Researchers don't know why some women develop gestational diabetes. To understand how gestational diabetes occurs, it can help to understand how pregnancy affects your body's glucose processing.
Your body digests the food you eat to produce sugar (glucose) that enters your bloodstream. In response, your pancreas — a large gland behind your stomach — produces insulin. Insulin is a hormone that helps glucose move from your bloodstream into your body's cells, where it's used as energy.
During pregnancy, the placenta, which connects your baby to your blood supply, produces high levels of various other hormones. Almost all of them impair the action of insulin in your cells, raising your blood sugar. Modest elevation of blood sugar after meals is normal during pregnancy.
As your baby grows, the placenta produces more and more insulin-blocking hormones. In gestational diabetes, the placental hormones provoke a rise in blood sugar to a level that can affect the growth and welfare of your baby. Gestational diabetes usually develops during the last half of pregnancy — sometimes as early as the 20th week, but generally not until later.
Gestational diabetes usually starts halfway through the pregnancy. All pregnant women should receive an oral glucose tolerance test between the 24th and 28th week of pregnancy to screen for the condition. Women who have risk factors for gestational diabetes may have this test earlier in the pregnancy.
Once you are diagnosed with gestational diabetes, you can see how well you are doing by testing your glucose level at home. The most common way involves pricking your finger and putting a drop of your blood on a machine that will give you a glucose reading.
To know more about Complications of GDM and its effect on Baby & Mother, and how to conquer GDM by L-Carnitine read second part of this Blog.
You may have a greater risk of developing gestational diabetes if you:
- Are obese when you become pregnant
- Have high blood pressure or other medical complications
- Have given birth to a large (greater than 9 pounds) baby before
- Have given birth to a baby that was stillborn or suffering from certain birth defects
- Have had gestational diabetes in previous pregnancies
- Have a family history of diabetes
- Come from certain ethnic backgrounds, including African, Hispanic, Asian, Native American, or Pacific Islander
- Are older than 30
But half of women who develop gestational diabetes have no risk factors.
What are the symptoms of gestational diabetes?
Gestational diabetes typically does not cause any noticeable signs or symptoms. This is why screening tests are so important. Rarely, an increased thirst or increased urinary frequency may be noticed.
Causes of gestational diabetes
Researchers don't know why some women develop gestational diabetes. To understand how gestational diabetes occurs, it can help to understand how pregnancy affects your body's glucose processing.
Your body digests the food you eat to produce sugar (glucose) that enters your bloodstream. In response, your pancreas — a large gland behind your stomach — produces insulin. Insulin is a hormone that helps glucose move from your bloodstream into your body's cells, where it's used as energy.
During pregnancy, the placenta, which connects your baby to your blood supply, produces high levels of various other hormones. Almost all of them impair the action of insulin in your cells, raising your blood sugar. Modest elevation of blood sugar after meals is normal during pregnancy.
As your baby grows, the placenta produces more and more insulin-blocking hormones. In gestational diabetes, the placental hormones provoke a rise in blood sugar to a level that can affect the growth and welfare of your baby. Gestational diabetes usually develops during the last half of pregnancy — sometimes as early as the 20th week, but generally not until later.
Exams and Tests
Gestational diabetes usually starts halfway through the pregnancy. All pregnant women should receive an oral glucose tolerance test between the 24th and 28th week of pregnancy to screen for the condition. Women who have risk factors for gestational diabetes may have this test earlier in the pregnancy.
Once you are diagnosed with gestational diabetes, you can see how well you are doing by testing your glucose level at home. The most common way involves pricking your finger and putting a drop of your blood on a machine that will give you a glucose reading.
To know more about Complications of GDM and its effect on Baby & Mother, and how to conquer GDM by L-Carnitine read second part of this Blog.




You there, this is really good post here. Thanks for taking the time to post such valuable information. Quality content is what always gets the visitors coming. مرض السكري والحمل
ReplyDeleteVery nice article. Just read Best Diabetes Doctor in Gurgaon And if you are looking for <a href="https://dharmadiabetesclinics.com/best-diabetes-doctor-in-gurgaon/</a>
ReplyDeleteand book your appointment for today..